The American Association of Diabetes Educators Annual Conference
The Beyond Type 2 team attended the American Association of Diabetes Educators (AADE) annual conference in Houston from August 8th to 12th. Diabetes educators, nurses and other health professionals gathered to present their latest research and discuss the current challenges and achievements in the diabetes industry. The sessions covered a variety of topics such as diet and nutrition, culture, peer support, mental health, technology and improving clinical standards of practice that impact people with type 1 and type 2 diabetes and other forms of diabetes. Sessions were organized to fit under the six pillars of AADE’s Project Vision, a new multi-year initiative to rebrand and expand the expertise of  diabetes educators. The six pillars are:
diabetes educators. The six pillars are:
- Drive integration
- Promote Person-Centered Care
- Include Related Conditions
- Focus on Behavioral Health
- Achieve Quadruple Aim
- Leverage Technology
One of the major changes announced at the conference was the name change from “certified diabetes educators” to “diabetes care and education specialists” to better reflect what diabetes educators do on a regular basis. At the opening general sessions, AADE President, Karen Kemmis, stated: “Diabetes education does not comprehensively capture what we do. In fact, within the health care environment, it sells us short and misrepresents what we have to offer systems, people with diabetes, providers and the entire care team. We know that our services are underutilized, and there are so many reasons for this, but our name is one part of it.”
At the event, we attended sessions of interest to people with type 2 diabetes such as the organization’s perspective on the ADA’s nutrition therapy consensus, peer support, stigma and more. Check out the highlights of the sessions we attended below!
ADA 2019 Nutrition Therapy Consensus
Earlier this year, the American Diabetes Association updated its nutrition therapy guidelines in its standards of care. These three-part sessions at AADE examined how these new standards can be applied in real-life settings and how diabetes care and education specialists should approach nutrition therapy with their patients.
One of the speakers, Janice MacLeod, remarked one of the top questions she gets from her patients is “What can I eat?” The answer to that? There is no one-size-fits-all solution to nutrition; nutrition and food choices are personal. However, she noted patients bring the expertise from their lives when figuring out the best meal pattern and professionals should meeting patients where they are. The four goals of nutrition therapy are:
- Promoting and supporting healthy eating patterns
- Address individual needs, including cultural preferences, health literacy and access to healthy foods
- Maintain the pleasure of eating
- Provide people with diabetes with practical tools to meal plan
Also, every person in a healthcare team should know and champion nutrition therapy and its benefits. Medical nutrition therapy (MNT), nutrition counseling and care provided by an  RDN, can help reduce A1c by up to 2 percent in people with type 2 diabetes.
RDN, can help reduce A1c by up to 2 percent in people with type 2 diabetes.
The session also covered the roots of our perception of nutrition and food. Alison Evert, another presenter, discussed the challenges in nutrition research such as all of us, including our patients, are hard-wired with our dietary patterns from birth and develop some of the habits of our parents. Think about it—what is a food or attitude towards food and nutrition you’ve held on to since childhood? More than likely, your feelings and attitudes were influenced by your environment. Evert dropped a couple of gems, too, by saying that “people don’t eat macronutrients, they eat food” and people live their lives with food, which means dietary planning shouldn’t be more stressful than it needs to be.
Health professionals most definitely shouldn’t be threatening their patients with insulin, either. By the time diabetes is diagnosed, 50 percent of beta-cell function has been lost. In type 2 diabetes, a progressive disease, beta-cell decline and insulin resistance are no one’s fault.
Christopher Gardner, an expert of study design from Stanford, discussed the oversimplification of nutrition news geared toward general audiences. When it comes to consuming information about nutrition and health, always be critical of the study you’re reading, including understanding the design and implications of the study.
45 million Americans go on diets every year and most fail to meet their goals. With that said, health professionals should help their patients set realistic goals and emphasize eating patterns. For example, if a patient is going to eat grains, emphasize whole grains. Though the consensus report evaluated the Mediterranean diet, vegan/vegetarian diet, low-fat diets, DASH diet, paleo diet, intermittent fasting and more, the evidence doesn’t support a clear preference for a specific eating pattern—we are all different.
Access to Insulin: Cost Drivers and Non-Medical Switching
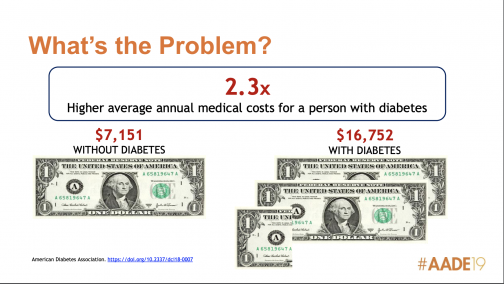
A highly-anticipated and engaging talk presented by George Huntley and Stewart Perry of the National Diabetes Volunteer Leadership Council about the barriers to insulin access and the higher costs of switching patients to new formularies but receive the same drug. This session began with a staggering stat —the annual cost of health care is 2.3 times higher for people with diabetes, who spend $16,000 than the general population at $7,100.
There’s a rising financial burden on people with diabetes plus more restrictions to access. Between 2008 and 2016, the average price of brand-name drugs increased by 208 percent. Meanwhile, from 2014 to 2016, the number of drugs on the exclusion lists of the two largest pharmacy benefit managers rose 65 percent. An outcome of this was non-medical switching, where a pharmacist will provide one brand over another, even if it’s the same drug or force the patient to take a less-expensive drug. This happens when prescription drug coverage changes are made. Non-medical switching can disrupt a person with diabetes’ (PWD’s) diabetes treatment plan and reduce its effectiveness by increasing frustration, increase out-of-pocket costs and increase the chances of side-effects.
Huntley and Stewart also covered the systemic problems within the health system that make insulin unaffordable: lack of transparency of pricing and rebates, the increasing use of high deductible health plans and a combination of medical and pharmacy deductibles. It begs the question, what is covered vs. what’s actually best for the individual?
Read Beyond Type 1’s Focus on Access to learn more about this issue.
Reducing Stigma to Improve Outcomes
Stigma can manifest itself in many forms, including racial/ethnic and other factors. This can result in health disparities, cause stress, the loss of social support and reduce one’s willingness to seek or obtain the care they need to improve their health outcomes. If you have diabetes, then you know the stigmas people with it face. In these sessions, we learned to reduce stigma to improve health incomes are being discussed by people in three stigmatized groups—legally blind, transgender individuals and people experience weight stigma. Presenters also defined shame and how it’s exacerbated in our current culture and society.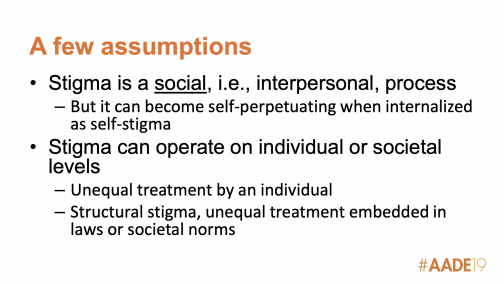
Eileen Ley, a legally blind (not diabetes-related) mother and wife to two people with type 1 diabetes, shared the story of her husband Tom, who went blind from diabetes at the age of 17. Her husband faced stigma from doctors, including one who stated they had no confidence in Tom to operate an insulin pump. Eventually, Tom managed diabetes so well no one else needed to be involved, however, Ley noted diabetes educators were his biggest advocates. When their son was diagnosed at the age of 4 with type 1 diabetes, Eileen had to learn how to manage his diabetes as a blind mother. She noted the benefits of accessibility features built into Apple devices that have made it easier to use tech like continuous glucose monitors (CGMs) and insulin pumps. However, Ley said there are ways to promote inclusivity for blind people with diabetes:
- Nag the industry to bring change
- Improve the accessibility of materials/resources such as large print, audio and digital handouts for people who don’t see well.
- Teach blindness etiquette/training.
- Get to know someone who’s blind + lives with diabetes.
 Next, Tristan Conor Murphy, a trans man with type 2 diabetes and firefighter, spoke about the challenges of being LGBTQ+ living with diabetes and working in healthcare. During his discussion, he said he witnessed colleagues misgender and mistreat trans patients. Feelings of being “othered” by doctors and colleagues can have a detrimental effect not just on blood sugar due to extra stress, but also prevent trans people with diabetes from calling for medical help in the event of an emergency. In regards to social support, Murphy has heard colleagues and friends say hurtful things behind his back which causes him to feel isolated and unwilling to socialize. Murphy emphasized ways to be more inclusive with LGBTQ+ people with diabetes:
Next, Tristan Conor Murphy, a trans man with type 2 diabetes and firefighter, spoke about the challenges of being LGBTQ+ living with diabetes and working in healthcare. During his discussion, he said he witnessed colleagues misgender and mistreat trans patients. Feelings of being “othered” by doctors and colleagues can have a detrimental effect not just on blood sugar due to extra stress, but also prevent trans people with diabetes from calling for medical help in the event of an emergency. In regards to social support, Murphy has heard colleagues and friends say hurtful things behind his back which causes him to feel isolated and unwilling to socialize. Murphy emphasized ways to be more inclusive with LGBTQ+ people with diabetes:
- Use clear, non-discrimination policies, especially for employees/patients.
- Self-honesty with own biases + getting to know someone who’s LGBTQ+.
- Use the right pronouns to avoid misgendering.
- Have all-gender bathrooms.
- Inquiring about relationship status, not just marital status.
- Calling them by their chosen name, even if it’s not on their birth certificate or medical records.
The third presenter, Laurie Klipfel, spoke about weight stigma and how she faced the worst bias from an orthopedic doctor when her knees were collapsing at age 56. Instead of performing an examination to determine the cause of her knee problems, the doctor automatically attributed it to her weight and advised her to lose it. After visiting another doctor, she received an MRI that revealed her knees were dislocated. She urged health care professionals to not focus too much on weight, but the benefits of healthy behavior with or without weight loss and avoid using “obesity”, a stigmatizing word, as a descriptor. In her words, “weight loss is not a behavior.”
Peer Support
Peer support was a major theme at this year’s AADE conference. One of the most important things about living with diabetes is finding someone who understands what you’re going through. Peer support in diabetes care can make a world of a difference. By finding common ground with others similar to you, you can help your diabetes and overall health goals can become more achievable. We’re covered several sessions about the usage of social media and online and in-person peer support in underserved populations. A few of the speakers at these sessions included Cherise Stockley of DiaTribe, Ashley Ng of Beta Change, Michelle Litchman and Heather Walker.
Finding a support group within the various diabetes online communities can influence a sense of empowerment and knowing there’s a shared experience with others. Some of the underserved groups of people with diabetes include people living with other disabilities and other diabetes-related complications. Walker stated people who suffer from complications are on the margins of peer support communities.
Litchman added diabetes support groups don’t necessarily have to revolve around diabetes, but instead be a group of people with diabetes who share a common interest. In regards to misinformation being spread in various groups, she said people in support groups are able to police themselves. Stockley emphasized the need for communities of color to be able to use their voices to share their experiences living with diabetes. According to Ng, people with diabetes also want more engagement from healthcare providers in the online space. Health providers can help their patients find peer support by creating their own resources and groups or finding others throughout the community and online.
“May the network be with you.”
No One Understands Me—Helping People Live Well w/ Diabetes
Who’s looking out for the emotional well-being of people with type 2 diabetes? Only 32 percent of people with diabetes can recall being asked that question by someone in their healthcare team. In this session living empowered with diabetes, the impact of diabetes distress and how professionals should respond to behavioral issues and concerns presented by their patients were explored.
Understanding a person with diabetes’s immediate needs and which behavior changes are hardest to change and why are critical in the first steps of diabetes treatment. In this session, educators and other professionals were urged to help patients talk about their feelings. People with diabetes could use help with even the smallest of changes and if there’s a failure to reach a goal, it’s not that patients aren’t “trying” or aren’t “compliant”—but instead, there could be other effects of diabetes distress at play. Use reflective listening and proper coping techniques. People most likely to suffer from diabetes distress are:
- Women
- Minorities
- People who lack insurance/underinsured
 Creating Lasting Behavioral Change in African-Americans with Diabetes
Creating Lasting Behavioral Change in African-Americans with Diabetes
African-Americans/Black people in the United States are disproportionately affected by type 2 diabetes and have one of the highest rates. Sharon Hawks, CEO, and director at the Nutrition and Education Center in Prince George’s County, Maryland addressed the cultural factors and barriers to diabetes self-care management, including seven stages of growth to behavior change:
- Dissatisfaction
- Vision
- Process
- Will
- Action
- Evaluation
- Recommit
The higher the income, the better one’s health tends to be, however, Hawks mentioned that’s not the case with Black/African-Americans in the United States. In Prince George’s County, African-Americans represent nearly 65 percent of the population and have the highest income-per-capita, yet the diabetes rate in Maryland is nearly 10 percent.
“In order to make a change, you gotta be sick and tired of being sick and tired,” said Hawks as she discussed the first stage of change, Dissatisfaction. She continued to explain the importance of identifying the strengths and setting goals, encouraging motivation and identifying obstacles, frequent follow-ups, being flexible according to your patient’s needs and recommitting to why the behavior change needs to happen.
Diabetes Devices: CGMs, Connected Devices and Insulin Pumps
Access to the latest diabetes tech can make management simpler. In these sessions about new diabetes devices, speakers are examined:
- The benefits of CGM therapy and why now is the time to use them, including promoting awareness and how educators can use them in their practices.
- New devices on the market and how certified diabetes educators (CDEs) can better leverage their use, and therefore improve the impact of a CDE’s work with patients.
- Preparing people with diabetes to use an insulin pump, as well as how peer support can help people with diabetes adapt to new diabetes technology.
One of the major highlights of these sessions came from Dana Hrobar, a CDE from Texas Children’s Hospital, who revealed a new model of introducing a CDE at the beginning of the CGM adoption process for patients. Diabetes care and education specialists can help interpret CGM data, discuss which behavioral changes the patient wants to make and refer those recommendations to the endocrinologist who can handle the technical aspects of an exam visit. This model increases the productivity of doctor’s visits, fewer issues in-between visits and improved target ranges.
Understanding Financial Access Barriers in Diabetes: Rationing and Underground Trading
This session tackled the increasingly important reality of the underground diabetes trading “black market”. As more and more people are left unable to afford diabetes supplies, where do they turn? And what is the outcome for these people seeking alternative treatments? Another important discussion topic is to what extent health care professionals and diabetes educators should be aware and able to advise on alternative methods of obtaining unaffordable medications. Presenters in this session include Michelle Litchman Ph.D., FNP-BC, FAANP, assistant professor and nurse practitioner at the University of Utah College of Nursing and Heather R. Walker MS, research analyst, Ph.D. candidate at the University of Illinois at Chicago. Click here to read our full coverage of this session.
Disclaimer: The American Association of Diabetes Educators (AADE) is a Founding Partner of Beyond Type 2.





