Research Suggests Changing Treatment Approach for Type 2 Diabetes
Written by: Liz Cambron-Kopco
4 minute read
May 24, 2022
With more medication and technology available for treating type 2 diabetes, it's about time more providers make better use of them.
During the 2022 Advanced Technologies and Treatments for Diabetes Conference (ATTD), researchers gathered to discuss new clinical frontiers of managing type 2 diabetes. The panels of experts discussed topics surrounding using holistic approaches for management, the benefits of early intervention and how to improve patient outcomes.
Why do current management practices need to change?
The current management practices tend to focus too much on just one aspect of diabetes management such as only A1C or weight loss, explained Stefano Del Prato, M.D.
Many current practices may wait too long to take more aggressive action—also referred to as “clinical inertia”—with medications and technology which puts people with type 2 diabetes at higher risk for developing complications.
Consequences of delaying more aggressive treatment include:
- People with diabetes have double the risk for heart attacks and cardiovascular disease (CVD), especially with higher A1C levels.
- Teens with type 1 diabetes and acute hyperglycemia have shown lower school performance due to cognitive impairment.
- Having elevated blood glucose levels is dangerous to the brain and cardiovascular system.
- Therapies are based on A1c measurements, which may not be accurate or show the full picture of a person’s blood sugar levels.
Dr. Del Prato emphasized that diabetes management should shift toward a more holistic approach, focusing on multiple goals to reduce the risks of complications.
What are the benefits of changing management practices?
“We need to change the philosophy,” stated Tadej Battelino, M.D., in his presentation on the benefits of early intervention.
In the STENO-2 trial, when placed on early intensive therapy, the risk for CVD in people with type 2 diabetes was reduced by 53 percent. This early intensive therapy tackled all CVD risk factors, not just one.
Having better glycemic control in the first 10 years of diagnosis led to a 33 percent reduction in the risk of CVD and a 54 percent reduction in nephropathy, suggesting that early intervention with intensive therapy is better long term.
What types of changes can be made?
Several strategies could be potentially effective, but most experts involved in this research agreed on two in particular.
Discuss and set goals with patients
“We should agree on a goal with a person with diabetes. It should be a goal that a person feels comfortable with and safe with. It’s a moveable target,” Dr. Batellino stated.
Managing type 2 diabetes can no longer be one-sided. Providers need to start engaging patients and include them in the decision-making process of their own care. Using appointment time to go through records and goals together is going to be key in making sure people with diabetes are knowledgeable and comfortable with any changes to their diabetes management.
“We want to help people see how their efforts are making a difference,” William H. Polonsky, M.D., said when discussing going over continuous glucose monitor (CGM) reports with patients.
By taking the time to compare past and current numbers, providers can show patients that their hard work and treatments are making improvements. This small change can make a huge difference when it comes to diabetes burnout and frustration.
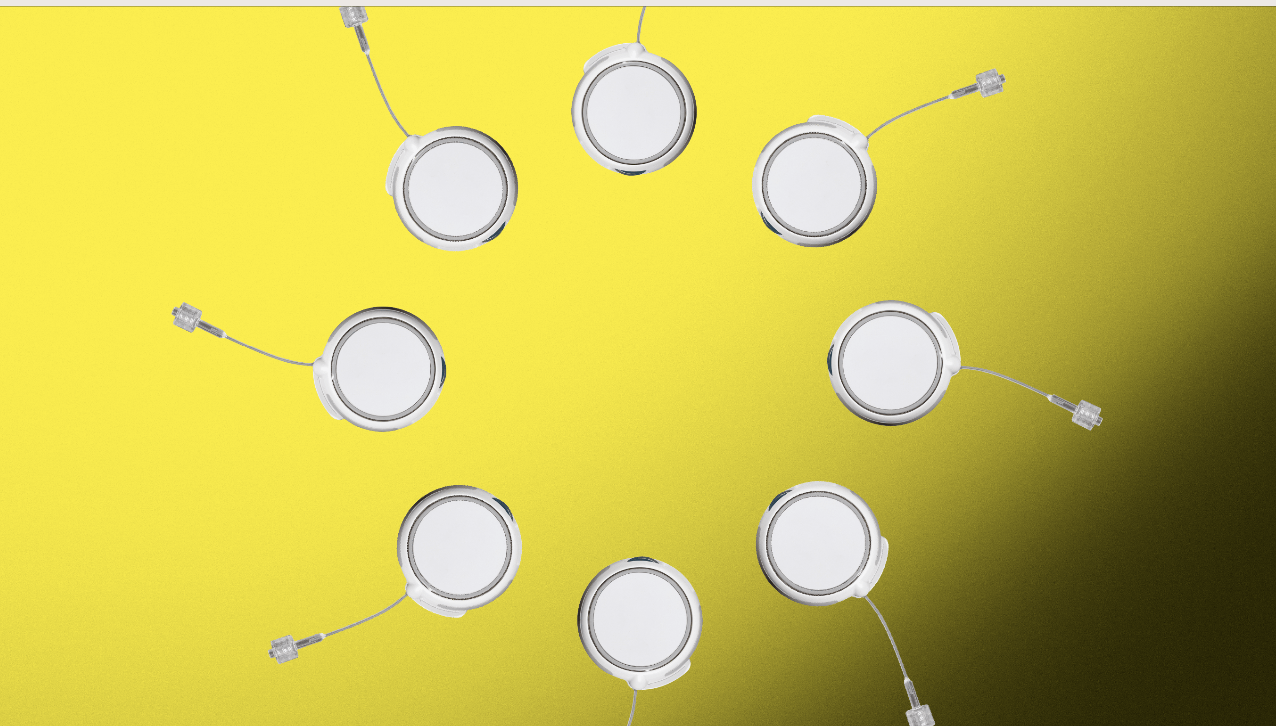
Utilize CGMs
The American Diabetes Association has recommended that all people with diabetes be offered a CGM, but only 10 to 15 percent of people with type 2 diabetes in the U.S. are using this life-changing technology.
How providers utilize the data from CGM technology has also not changed.
Richard Bergenstal, M.D., emphasized that providers need to not only know how to quickly read CGM data but should also start interpreting the data to create an action plan with the following guidance:
- More Green: Make changes to increase time in range (TIR)
- Less Red: Reduce the number of hypoglycemic events
- FIR: Keep graphs flat and in target ranges
However, CGM data isn’t just for providers to interpret. Steven V. Edelman, M.D. brought up the importance of patients knowing how to understand and interpret their own CGM. Providers need to make sure that patients know and understand the trend arrows and how to use the alarms.
It’s important for people with type 2 diabetes to understand how to read trend arrows to make behavioral changes—like when to take insulin or when to treat for an oncoming low.
Small changes could make a big difference
Some other suggested changes for the future of diabetes management included:
- Introduce efficient medication earlier on after metformin to prevent complications
- Using virtual diabetes clinics to overcome access barriers
- Have a connected care system (patient portal) so all providers and the patient have access to the same information.
- Try new medications like dual agonists.
- Speak in lay terms (ex: explain hours per day in range versus a TIR percentage).
Overall, experts in this research agree that diabetes management needs to shift to a patient-first focus, through personalized care. When people with diabetes feel heard, their diabetes management improves.
You are part of your diabetes management team too.

Author
Liz Cambron-Kopco
Liz has been living with type 2 diabetes since 2014, but grew up surrounded by it as a first-generation Mexican-American. With a bug for research, Liz pursued a PhD in molecular biology and spent her early career studying insulin signalling in invertebrates to understand how insects' tiny little bodies work. Along with advocating for women and girls in STEM, Liz shares her personal journey with diabetes on her social media platforms to help teach people to become their own advocates. Her passion for advocacy led her to join the Beyond Type 1 team. When she's not advocating, Liz enjoys hiking with her husband and their terrier/schnauzer mixed pup Burberry.
Related Resources
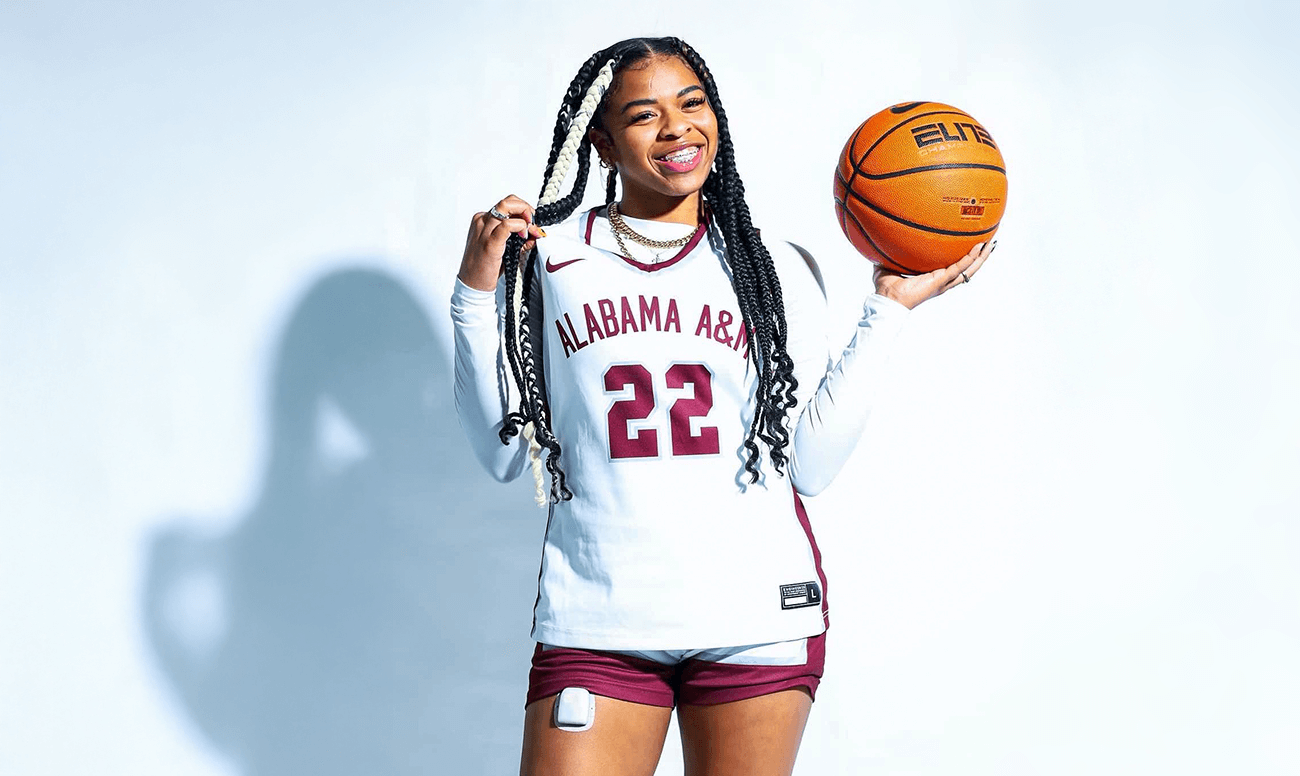
When 13-year-old Shelomi Sanders had a stomach ache, she never imagined it signaled a life-changing...
Read more

Hyperglycemia—or high blood sugar—can sneak up on you, whether it’s from a missed dose, a...
Read more
Sequel just announced big news for people living with type 1 diabetes: Its twiist automated insulin...
Read more

