People With Diabetes Forgoing Basic Needs in Order to Survive According to New Studies
Written by: T'ara Smith
4 minute read
August 11, 2019
According to two studies presented at the American Association of Diabetes Educators 2019 Annual Conference, people with diabetes are forgoing basic needs in the face of rising healthcare costs and taking to underground exchanges of necessary supplies.
According to two studies presented at the American Association of Diabetes Educators 2019 Annual Conference, people with diabetes are forgoing basic needs in the face of rising healthcare costs and utilizing alternative methods for procuring necessities for their care. Skyrocketing out-of-pocket costs and deductibles coupled with the increasingly prevalent issue of affordability of supplies and medications like insulin has prompted a number of people with diabetes to partake in underground exchanges of necessary supplies.
Over the course of these studies, which were presented by lead author Michelle Litchman, Ph.D., FNP-BC, an assistant professor at the University of Utah College of Nursing, researchers surveyed 159 adults affected by diabetes, including caregivers and care partners. Findings concluded that nearly half of the individuals  who participated cannot afford necessities for their family as a result of the costs of their condition. The financial distress faced by the diabetes population forces some to go without reliable food, clothing, shelter and transportation. Rationing doses of medication, reusing diabetes tools and skipping blood sugar tests were also common among those examined in the study. While assistance from pharmaceutical companies is available, only 58 percent of people who apply actually receive it.
who participated cannot afford necessities for their family as a result of the costs of their condition. The financial distress faced by the diabetes population forces some to go without reliable food, clothing, shelter and transportation. Rationing doses of medication, reusing diabetes tools and skipping blood sugar tests were also common among those examined in the study. While assistance from pharmaceutical companies is available, only 58 percent of people who apply actually receive it.
Quoting a participant from the study, Litchman said: “‘I had to pay rent, but instead I needed insulin.” Litchman calls this the debt or dead dilemma—patients who have to make decisions between their life-saving medication or basic life necessities. Referencing to another patient, Litchman added: “ For some patients, some days they can only eat rice and ramen, meat is a luxury. How can we ask our patients to eat healthy foods if they can’t even afford it?”
Researchers also documented the existence of an underground exchange system commonly utilized by people with diabetes and their caregivers. Those in need trade, borrow and purchase medications and supplies to bypass the rising costs of their healthcare. These purchases are made from unauthorized and illegal diabetes suppliers. More than half of study participants admitted to having donated to others in need, while a third of the study population said they had received a donation. The data suggests the system is preventing hospitalization and death while bypassing common delays of healthcare bureaucracy.
The study showed that people living with diabetes were affected whether or not they had health insurance. Those who experience financial distress are nearly seven times more likely to engage in trading and nearly three times more likely to engage in receiving donations.
Listed in the session were the benefits and consequences of underground exchange activity:
Benefits:
- Prevented hospitalization and death. People with diabetes decide to purchase supplies from an unauthorized supplier over going to the ER, where they know their healthcare costs will go up.
- Preventing delays in care. Fewer or no time wasted on waiting to be seen by a professional.
- Ability to try before you buy. People with diabetes can temporarily try a new product without going through their insurance.
Consequences:
- Financial burden. Sharing supplies with another person can force the donator to purchase more supplies sooner than usual. Most wouldn’t share their supplies unless they absolutely could, however, they’re more likely to share their supplies with family members. Those who have an excess of diabetes supplies will donate it to those in need and wait to collect an excess of supplies before donating further.
- Potential safety issues. Some will knowingly take insulin that’s not refrigerated, test using expired test-strips, or even use continuous glucose monitor (CGM) sensors that don’t work. Places where people with diabetes purchase supplies include eBay, Craigslist and even going across the border.
Litchman revealed a part of these studies was that most surprised her: the impact of financial distress had on the siblings. “I was surprised about the effect it 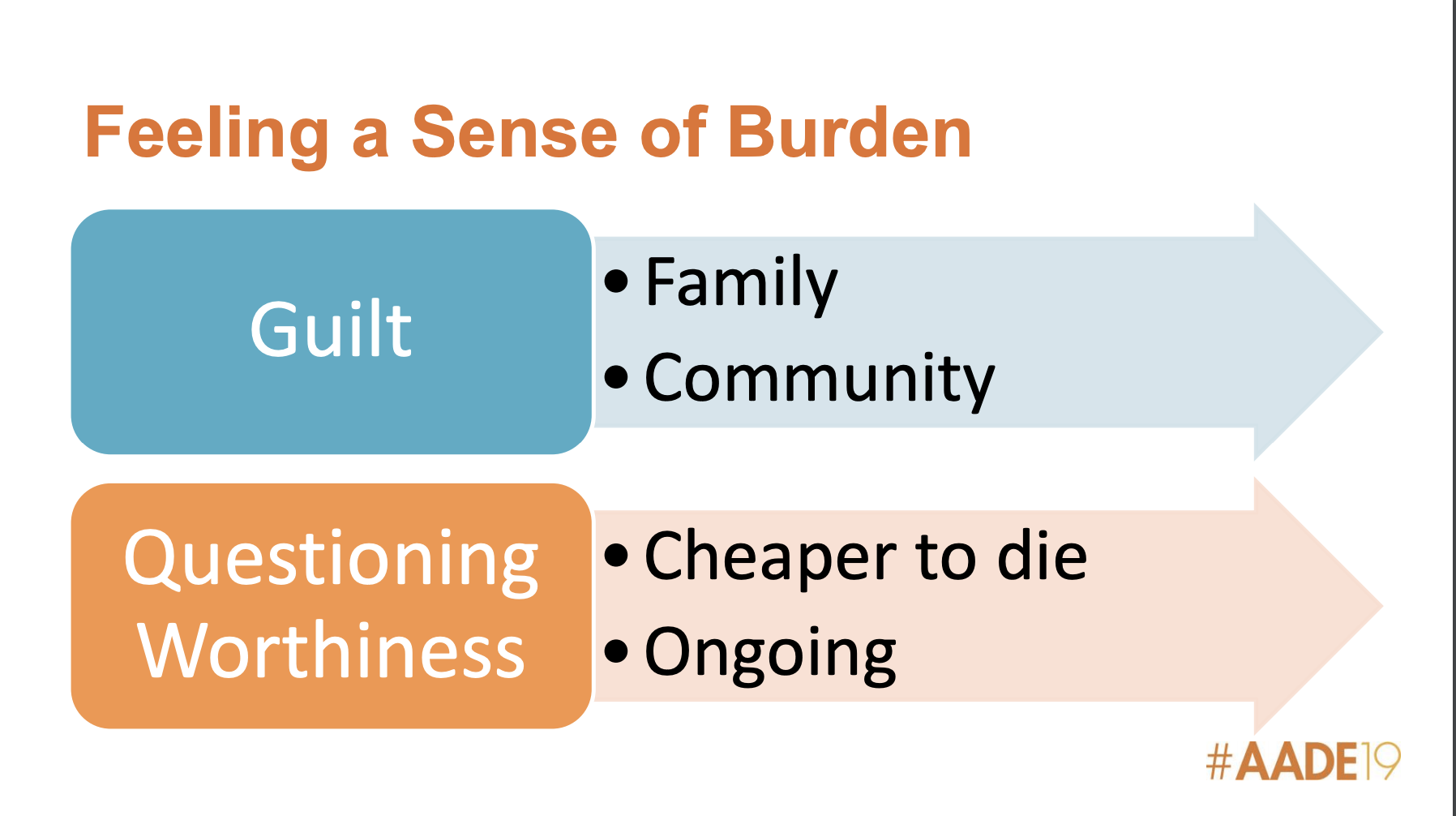 had on the siblings. There was resentment about the financial burden of costs of care, as well as the guilt of the parents who had to pay for the treatment,” said Litchman. Feeling a sense of financial burden is the result of feeling guilty that a person with diabetes has a condition that’s financially draining. Other examples shared during the session was a patient stating it would be cheaper to die. Litchman noted the patient wasn’t suicidal; they were just stating a fact about their life.
had on the siblings. There was resentment about the financial burden of costs of care, as well as the guilt of the parents who had to pay for the treatment,” said Litchman. Feeling a sense of financial burden is the result of feeling guilty that a person with diabetes has a condition that’s financially draining. Other examples shared during the session was a patient stating it would be cheaper to die. Litchman noted the patient wasn’t suicidal; they were just stating a fact about their life.
Is Underground Trading a Worsening Issue?
Litchman says yes, especially among those who are on insulin and those who don’t know how to use or access technology, an issue that also greatly impacts people with type 2 diabetes. One in four couldn’t use diabetes technology even if they wanted to.
The repercussions of high insulin prices can be deadly—There have been a troubling number of stories lately regarding deaths related to insulin prices. It was recently reported that Josh Wilkerson died after aging out of his stepfather’s insurance plan and switching to a more affordable type of insulin. Just last month, the family of 21-year-old Jesimya David Scherer-Radcliff shared that he died as a result of rationing his insulin. Similarly, 24-year-old Jada Louis passed away in June after a week-long hospital visit to treat diabetic ketoacidosis (DKA), brought on by her skipping insulin doses. In 2017, Alec Smith, Antavia Lee-Worsham and Justin Lutgen all died after they could no longer afford insulin and began rationing.
When discussing what diabetes educators and care specialists can do address the issue, Litchman said patients need to be asked if they’re engaging in this behavior because professionals need to know how to educate and assess the safety of the supplies they’re using.
“People don’t want to be fraudulent or break the law. People want to be well. We need to recognize this is why they started this anyway,” said Litchman.
If you or someone you know is having trouble accessing insulin, click here.

Author
T'ara Smith
T’ara was diagnosed with type 2 diabetes in July 2017 at the age of 25. Since her diagnosis, she focused her academic studies and career on diabetes awareness and living a full life with it. She’s excited to have joined the Beyond Type 1 team to continue her work. Two years later, T'ara discovered she'd been misdiagnosed with type 2 and actually has latent autoimmune diabetes in adults (LADA). Outside the office, T’ara enjoys going to the movies, visiting parks with her dog, listening to BTS and cooking awesome healthy meals. T’ara holds an MS in Nutrition Education from American University.
Related Resources

Already compatible with Dexcom’s G6 and G7 continuous glucose monitors (CGMs), the Omnipod 5 Automated...
Read more

The younger a person is diagnosed with type 2 diabetes, especially those with obesity, the...
Read more

The Oura Ring, which tracks things like sleep, heart rate, and activity, is joining forces...
Read more

