Ask a CDCES: Why Should I Change My Insulin Injection Sites?
Written by: Jodi Lavin-Tompkins MSN, RN, BC-ADM, CDCES
5 minute read
March 27, 2020
Why should you change your insulin injection sites? Get your answer in our Ask a Diabetes Care and Education Specialist (DCES) column!
It can be easy to get into the habit of using the same area to inject insulin. But for a number of reasons, it’s important to rotate those injection sites periodically to make sure you’re using insulin effectively. A certified diabetes and education specialist (CDCES) from the Association of Diabetes Care and Education Specialists (ADCES) provided tips about how using the same injection site repeatedly can be detrimental to your self-management and the best ways to choose different sites on your body.
Dear CDCES: I notice my insulin isn’t bringing my blood sugar down to my normal range anymore. I always inject insulin in the same spot, could that be the problem? Should I change my injection site?
Dear Reader: This is a great question and I think the answer could help a lot of people with type 2 diabetes (T2D) who take insulin see a major difference in their blood sugar levels and overall diabetes management.
When you learned to take insulin, you may or may not have been encouraged to change your sites, but you may not fully understand why. Changing can mean:
- Moving from the stomach to the arm to the thigh.
- Moving over one inch from the last injection in the same area of the body.
Insulin causes the fat cells in the tissue of the injected site to grow. This means that over time, you may see extra fat in the areas where you inject. Too much of this fat leads to several problems and prevents your insulin from being absorbed normally. This condition is called Lipohypertrophy.
Why is it important to change insulin injection sites?
Giving injections in the same general area eventually leads to some numbness in that area. It is more comfortable and less painful for you to inject there. However, this is a sign that you probably have lipohypertrophy. This can lead to:
- Insulin not being able to be absorbed normally, which leads to higher blood sugar levels.
- The need to increase your dose of insulin over time in order to achieve your blood sugar targets (more insulin means higher financial costs).
- A higher risk for hypoglycemia when you do move your injection to a new site because the higher dose of insulin is absorbed optimally in the new area.
How do I know if I have lipohypertrophy?
The type of fat you develop with lipohypertrophy is different from the fat you see when you gain weight. If you may think you have lipohypertrophy, contact your health care provider. Signs and symptoms of lipohypertrophy include:
- A1c steadily going up and more ups and downs with your blood sugar level.
- Needing to increase your insulin dose without changing your usual routine.
- Your frequent injection site tends to be raised and circular, often the size of a small orange.
You may have to look in the mirror for a front and side view to see it clearly. If you’re having trouble picturing what it is supposed to look like, look no further than chipmunk cheeks for the size and shape that is common. Need an example? Look at the gentleman in the picture below who has severe lipohypertrophy.

Your degree of lipohypertrophy may be mild, moderate or severe. The milder it is, the harder it is to see. But knowing how often you use that particular part of your body for injections can give you the first clue.
For example, since guys often wear untucked T-shirts or button-down shirts, they tend to use either side of their belly button because it’s the easiest place to reach with just lifting or unbuttoning a shirt.
Below is a good example of someone who has only taken insulin for six months but is primarily injecting in those areas of his stomach and has mild lipohypertrophy. You may notice that one side has more fatty tissue than the other. This is because if you are right-handed, it is probably easier to give your injection on the right side, and vice versa.
 Preventing + treating lipohypertrophy
Preventing + treating lipohypertrophy
Research has shown that reusing pen needles contributes to lipohypertrophy. Most pen needles are designed for one-time use and get microscopic damage with every use. This promotes injury to the tissue with each injection even if you don’t feel it. Lipohypertrophy may go away but it could take weeks or months. But by avoiding those sites, you should see them shrink at least somewhat over time.
What is the best way to change sites?
The best method is whatever works best for you and helps you remember where you gave your last injection. Some people find that thinking of the body area you are using as a clock helps. Give the first injection at 12 o’clock, the second at 3 o’clock and so on. Others use imaginary lines going across the site and then moving down to the next imaginary line (horizontal pattern).
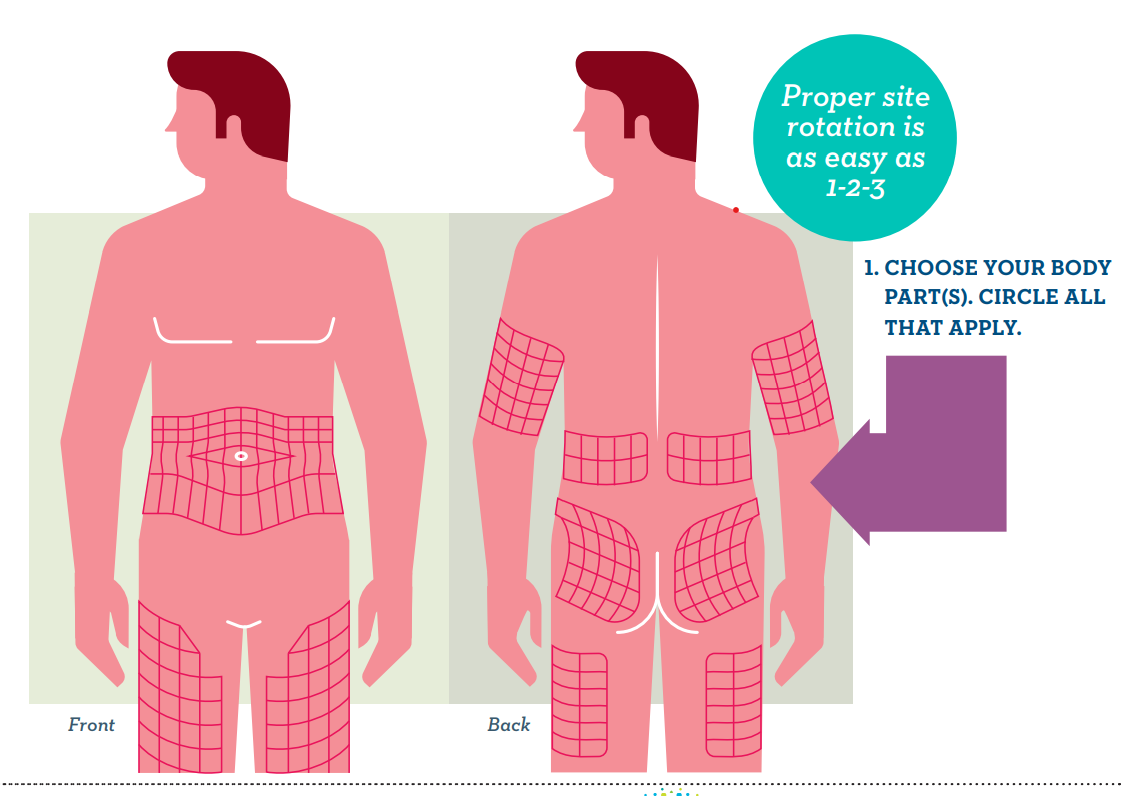
Others have gotten creative and developed their own patterns. It’s still better to use the areas outlined in the figure below for the best absorption. It’s also best to avoid injecting into scar tissue or areas where you can’t pinch an inch.
Pro-tip: Insulin absorption is different depending on where on your body you inject it. The best absorption happens when you inject in your stomach area, followed by arms, thighs and buttocks. It’s best to avoid injecting into a muscle, as it changes the action of the insulin.
The bottom line is if you need to take insulin, rotating your injection sites, using as much of the entire area of the body as possible and changing your needle for each injection can save you time, money and frustration by preventing lipohypertrophy from developing. You can do it!
Editor’s Note: This content was published in partnership with the Association of Diabetes Care and Education Specialists (ADCES), a founding partner of Beyond Type 2.

Author
Jodi Lavin-Tompkins MSN, RN, BC-ADM, CDCES
Jodi Lavin-Tompkins is a North Carolina native and a master’s prepared nurse with over 30 years’ experience in diabetes care. She is currently the director of accreditation/content development at the Association of Diabetes Care & Education Specialists. Jodi’s career has spanned working in academic settings as a nurse practitioner to positions in the pharmaceutical and medical device industries, to managing a diabetes self-management education and support program in a large midwestern health system. She is passionate about making sure people with diabetes have the knowledge and skills they need to manage diabetes to the best of their abilities. To Jodi, diabetes is personal; her mother, father, brother, niece, cousin, aunt and uncle all have diabetes.
Related Resources

There might come a time when you or your doctor want to try a new...
Read more

Editor’s note: This article includes Ginger’s personal experience taking metformin in addition to her daily...
Read more

Health insurance can be a headache, especially when selecting a plan that will cover the...
Read more

