How Smartpen Devices Help People with Type 2 Diabetes
Insulin pumps are not the only way to improve diabetes self-care for people with type 2 diabetes. Insulin pumps can be costly, barriers due to lack of insurance coverage, complexity and training needed to use it. Also, there are people with diabetes who don’t want devices attached to their body or prefer to only wear a continuous glucose monitor (CGM).
If you’re on multiple daily injections (MDI), this article is for you. At the Association of Diabetes Care and Education Specialists’ conference, we covered two sessions that discussed the benefits of smart insulin pens to manage diabetes. Currently, the only two on the market are the InPen and BigFoot Unity. The InPen can be integrated with Medtronic and Dexcom’s CGMs and BigFoot Unity’s smart insulin cap can be integrated with the Freestyle Libre.
Colleen Miller-Owen, APRN, CDCES, from the Tampa General Medical Group, discussed how smart insulin pens mimic insulin pumps. They offer similar features and functions such as:
- Bolus dose calculators: how much insulin is needed based on the number of carbs for a meal.
- Fixed-dose options: Meal estimations and set doses, great for people who don’t like carb counting.
- Correction doses: Based on insulin sensitivity factors and also considers how much active insulin is in your body (also called insulin-on-board).
- ½ unit delivery options
- Dose reminders
One of the burdens for people with type 2 diabetes on insulin is keeping track of how well your insulin regimen is actually working. This includes remembering how much insulin was taken, especially for meals or to lower high blood sugar. Fortunately, smart insulin pens relieve that burden and automatically capture data such as:
- Record the time of the insulin dose
- How much insulin was given
- Assess for missed doses
- Dosing behavior
- Use of the bolus calculator
- Assess basal/bolus percentages to determine if your insulin-to-carb ratios are correct and your basal doses are correct.
All of this information is collected into reports that can be downloaded directly on your phone and used for your doctor’s appointments. You can identify trends, areas of improvement and what’s working well.
Who’s a Smartpen Candidate?
Miller-Owen emphasized that any patient with diabetes needing insulin is a viable candidate and providers should be open to discussing smartpens for people who:
- Are on meal-time and correction-dose insulin
- Want to take a pump-break or need a back-up
- Need to better track their insulin dosages and carb intake
Real-World Experience with Smartpens
Miller-Owen cited her experiences with 17 of her own patients using smartpens and another nine patients who were prescribed one but didn’t use it. She says this shows smartpens are a viable option for people with diabetes on insulin.
Observation of 17 Patients Using Smart-Pens
- Seven improved their A1C
- Eight increased their A1C, but time-in-range improved from 39 percent to 67 percent
- Two increased their A1C but didn’t use calculator consistently
Observation of 9 patients who were prescribed a smartpen, but didn’t use it:
- Five increased their A1C
- Four improved A1C, but only one fell under 7 percent.
Use DATAA to Improve Your Next Doctor’s Visit
Diana Isaacs, PharmD, BCPS, BC-ADM, CDCES introduced the DATAA protocol to help doctor’s appointments be more efficient and data-driven by using connected care devices such as smartpens.
For example here’s the approach to DATAA, as described by Issacs:
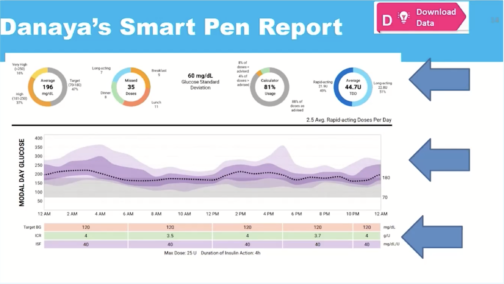
D – Download Data: Get a global overview of the data and discussing what you’ve learned.
A – Assess safety: identify time-in-range, hypoglycemic events and identify causes and solutions.
T – Time-in-Range: Focusing on the positive by identifying when you’re most within your targets and learning what’s working well for you.
A – Areas to improve: Identify that were above your blood glucose range and create solutions or adjustments to improve self-care.
A – Action Plan: Using all of the learnings above to create actionable steps.
DATAA Patient Example
Isaacs discussed a fictional patient scenario of a 65-year-old woman, named Danaya, with latent autoimmune diabetes in adults (LADA) diabetes who uses a smart insulin pen with a CGM. Her smart insulin pen has a carbohydrate counting feature along with insulin dosage recommendations. The recommendations list how much insulin you should take based on the number of carbs per meal. The recommendation is based on factors such as your insulin sensitivity factor and your carb-to-insulin ratio. In this example scenario, the patient’s blood glucose is higher after breakfast and she sometimes forgets to take insulin when eating a snack before bedtime, leading to higher fasting blood glucose levels. In addition to long-acting insulin, she also uses mealtime insulin.
Download Data
In Danaya’s assessment for long-acting insulin, Isaacs can see:
- Average daily insulin dose taken
- Missed dosages
- Number of days with blood glucose below 3.9 mmol/L70 mg/dL
- Median Bedtime to Fasting (how much blood glucose levels change during sleep)
Isaacs also noted when used optimally, long-acting insulin, assuming there’s no mealtime/bolus insulin given, should help blood glucose stay within 30 points.
For mealtime-insulin, Isaacs can view:
- How blood glucose changes during breakfast, lunch and dinner over a period of hours, based on how the patient logs their pre-meal and post-meal blood glucose levels.
- Missed dosages and dosages logged for specific meals
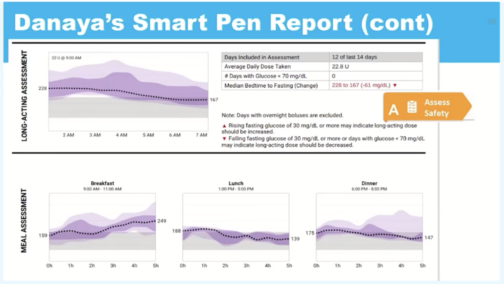
Assess Safety and Time-in-Range
Think a CGM always records low blood glucose events? Not always! Isaacs mentioned she always asks a patient if they experience low blood sugars and how they’ve been treated. However, as a patient, it’s important to notify your provider of any low events that may not show up on your data reports. After that, you and your provider can use the smart insulin pen’s time-in-range report to learn what’s working well. Some important ways to reinforce what’s working:
- Changes in exercise routines
- Tracking meals, including taking photos to remember what was eaten
- Improved insulin-to-carbohydrate ratio skills by using the bolus calculator
Areas to Improve and Take Action
For areas to improve, Danaya identified where she’d like to make changes:
- Forgetting to bolus/take mealtime insulin
- Needing to adjust carb ratios
- Identify possible reasons for not using the bolus calculator feature consistently
Using these factors, she and her provider turned them into an action plan:
- Continue using the same long-acting insulin dosages, but improve mealtime dosages by increasing insulin-to-carb ratios for breakfast.
- Either remove bedtime snacks or bolus for it
- Set reminders to bolus on the mobile app
A great thing about smartpens is, similar to a pump, you can adjust your carb-count ratios for different meals. For example, Isaacs mentioned if you’re usually running higher during and after breakfast time, you can adjust how much insulin you need specifically for breakfast.
Key Takeaways:
As a person with diabetes, having the seamless integration can help remove the burden of needing to manually enter data, but instead, have it collected and reported at once. Having better means having better data-driven conversations with providers. The goal of connected care devices is to provide diabetes care in a holistic, systematic fashion. They’re a viable alternative to insulin pumps and can be an important tool to optimize your care and your DCES or another healthcare provider can help you get connected.
This content was made possible with support from Lilly Diabetes, a Founding Partner of Beyond Type 2.





