Diabetes Care in Hospitals: An Update
The American Diabetes Association (ADA) included a review and update of intrahospital management of different types of diabetes in its guidelines and overall consensus of 2019. Both hyperglycemia and hypoglycemia are risks should be avoided, as they are often the cause of hospitalization in the first place.
Although this update includes a range of specific data on the use of medicine the information is designed for health professionals, it might be a good idea to meet with your healthcare team to discuss this information in case you require any hospitalization and would like to plan in advance!
General Recommendations
Some of the recommendations for proper management in hospital environments include some of the following:
- Glycosylated Hemoglobin—it is suggested that this test be performed on all admitted patients who report having a history of diabetes and who do not have on-hand results from the last three months or who are admitted with hyperglycemia (values higher than 7.8 mmol/L140 mg / dL).
- Diabetes Education—conducting a self-management assessment of diabetes knowledge is advised. If patients find they have little to no real knowledge of the condition, it’s vital to receive primary diabetes education before being discharged.
- Specialists in Charge—it is suggested that patients with diabetes admitted to a hospital environment receive care from a diabetes specialist or if that’s not doable, a multidisciplinary team that can be responsible for glycemic management of the patient.
- Blood Glucose Targets—insulin therapy should be initiated if hospitalization is due to elevated levels of sustained BGs with a minimum value greater than 10.0 mmol/L180 mg/dL. Once insulin therapy has started, the target ranges will be between 7.8-10.0 mmol/L140-180 mg/dL, but lower levels (6.1-7.8 mmol/L110-140 mg/dL) may be chosen if the patient is not at risk of hypoglycemia.
- Blood Glucose Monitoring Frequency—those patients in a hospital setting who can feed themselves should measure their blood glucose levels before and after food. In case the patient is not eating, monitoring should increase in frequency up to every two hours.
- Food in Hospital Environments—today we know that not all of us who live with diabetes (any type) follow the same nutritional plans. There are different plans and different individuals. In a hospital environment, recommendations are based on glycemic objectives. In some cases, you may request the intervention of a dietitian, nutritionist, or diabetes educator who can help with your meal plan.
Managing Steroid Induced Hyperglycemia
As you might remember, some meds will have an effect on our blood sugar levels. Such is the case for steroids (Prednisone for example).
Presenters mentioned the need of modifying insulin dosing in order to address these blood sugar spikes. Recommendations suggest adding units per kilo/ per day/ basal although we know that this decision will also depend on individual needs and patients blood glucose. NPH was used as an example for some clinical scenarios but other basal insulins were mentioned as well.
NPH Dosing example:
| Prednisone (mg/day) | NPH (units/kg/day) |
| 10 | 0.1 |
| 20 | 0.2 |
| 30 | 0.3 |
| above or equal 40 | 0.4 |
In a retrospective study of 58 non-critically ill patients with an equivalent of Prednisone of 30 mg per day those who achieved normoglycemia had an average total daily dose of insulin of 0.8 units per kilo per day. Between 30 and 35 percent of this daily total was basal insulin and between 65 and 70 percent prandial insulin.
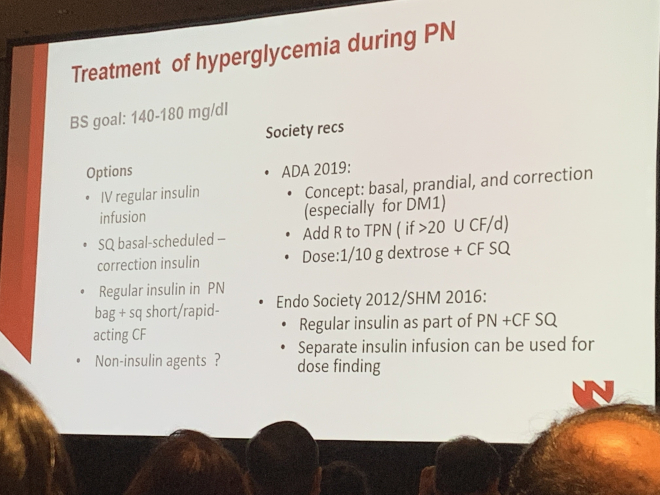
Managing Hyperglycemia During Inpatient Nutritional Support
It is recommended the use of prandial, basal and correction doses of insulin. Blood sugar goals in this case are 7.8-10.0 mmol/L140-180 mg/dL as avoiding hypoglycemia is a priority in this medical and clinical scenarios. Evidence shows hyperglycemia is a frequent complication of enteral and parenteral nutrition in hospitalizations. Managing hyperglycemia in these patients includes optimization of carbohydrate content and intravenous or subcutaneous insulin doses adjustments.
A reminder of General Guidelines for us; people with diabetes
Self-management? In some cases, the patient may be allowed to be in charge of managing their diabetes. The appropriate candidates for this scenario are those who have the knowledge, skills and abilities required to do so. The team of health professionals in charge will be the ones who decide if the patient will be able to do it on their own or not.
It is essential, as we mentioned, to consult these guidelines and discuss them with the team in charge of managing your diabetes. Planning before a hospitalization can make these moments less stressful. Diabetes education is the key to making better-informed decisions and avoiding hospital readmissions due to causes that may have been handled at home. We know that two plus two doesn’t always equals four when it comes to diabetes, but the more we know, the better decisions we can make, and these risks will be considerably diminished.
References:
American Diabetes Association. 15. Diabetes care in the hospital: Standards of Medical Care in Diabetes—2019. Diabetes Care 2019;42(Suppl. 1):S173–S181
This article is part of Beyond Type 2’s ADA 2019 coverage. For full ADA 2019 coverage, click here.





