What We Can Learn From Diabetes Care in India
Leading experts in diabetes care from India shared research and findings on the state of type 1 and type 2 diabetes care at the Advanced Technologies and Treatments for Diabetes (ATTD) 2022 conference.
India boasts a population of 1.36 billion people and approximately 74 million of those are living with diabetes—that’s more people than the entire population of France. By looking at the state of diabetes care in this country, researchers propose it could help improve diabetes care worldwide.
The research discussed included novel approaches to patient education, cost barriers to healthcare, and treating rural populations and those with few economic resources.
Understanding unique presentations of type 2 diabetes (T2D)
Diabetes, like many conditions, can not be treated as one-size-fits-all, and research out of India illustrates this well. The following is a synopsis of a presentation by Viswanathan Mohan, M.D., a leading diabetes doctor and researcher working in India.
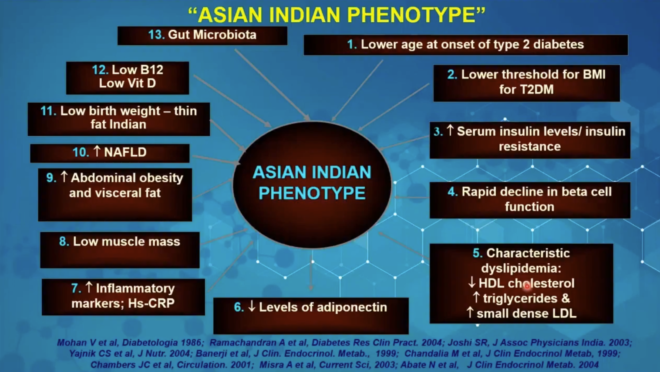
In India’s population, type 2 diabetes looks pretty different—the average age of onset is lower, obesity is less prevalent at diagnosis, and low HDL and high triglycerides are common features.
A recent Danish study identified and classified four common phenotypes, or profiles of genetic and clinical features, of type 2 diabetes. Interestingly, only two of those phenotypes were found in India, along with two separate, novel phenotypes.
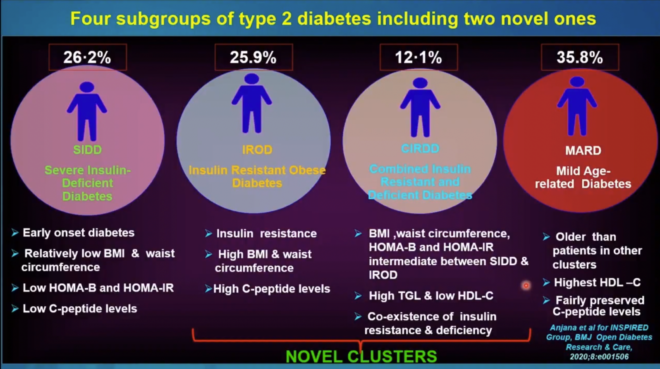
The extensive analysis of the way diabetes presents in India demonstrates how genetic differences and possibly other variables play a part in the development and progression of T2D.
For example, both Danish and Indian studies show certain phenotypes have greater risks for complications like retinopathy or chronic kidney disease.
Similarly, different phenotypes appear to have different likelihoods of achieving an A1C below 7%, a common treatment goal.
With this knowledge, the healthcare sector can offer more focused treatment and patient care.
Software that makes personalized diabetes care available anywhere
Dr. Mohan’s group has developed Diabetes Novel Subgroup Assessment (DIANA), a software tool that can be used in clinics anywhere in the country.
“Just by putting in the clinical parameters, the software will tell you which subtype of diabetes you have,” Dr. Mohan explained. These parameters include BMI, waist measurement, A1C, HDL and others.
This is an example of using data to create diagnostic tools that can be used by providers of different levels of resources or specialized training.
The software will also show risk profiles for different complications and what kinds of treatment are best suited for different subgroups.
Using telemedicine to increase access to healthcare providers
Kerala, a state in the southern part of the country, was the first country to recognize type 1 diabetes. A phone-based resource for diabetes management and support has been in place there for 25 years.
The support network uses the messaging service WhatsApp as a public forum where people can pose questions and interact with other users as well as doctors and providers.
The benefits include communicating with your healthcare team at any time, getting help making adjustments to medication dosage or troubleshooting devices between appointments.
This model is particularly beneficial for patients who pay out-of-pocket for all healthcare services and in regions where the may be a shortage of health care providers.
“During the Covid pandemic we have again realized that we can offer probably equivalent or better care—yes, even better care—and we can expect better outcomes in type 1 diabetes (T1D), not just in telemedicine but when telemedicine is practiced along with infrequent, face to face visits,” said Jothydev Kesavadev, who runs a diabetes research center in Kerela.
Benefits of accessing providers on digital platforms:
- Users can get questions answered any time of day.
- Providers could treat or avert hypoglycemic events.
- Dieticians could provide individualized guidance on dietary modifications.
- Non-emergency interventions reduce or avoid hospitalizations.
- Parents and children could get re-trained on injection techniques as needed.
- Users could ask questions about stopping insulin therapy, side effects, or alternative treatments and get detailed answers.
- Someone experiencing a shortage of supplies such as test strips or needles can be quickly connected to resources in their community.
- Troubleshooting devices or injection techniques over video
- The service is free.
Drawbacks:
- Doctors and providers do not have access to individuals’ medical records.
- If a person is on a treatment protocol that is inappropriate given their specific needs, providers cannot comment or change it.
- Many users will contact providers privately on Whatsapp, however, due to legal liability, providers cannot respond directly to.
- A group messaging forum isn’t the best place to address sensitive questions and concerns.
- The open forum isn’t secure or confidential.
- The service has no source of funding or revenue and there is no way to compensate providers for their time.
Addressing gaps in diabetes education
“Type 1 diabetes is an expensive disease to live with if you have to pay out of pocket like you do in India. There’s no healthcare scheme, there’s no insurance,” said Jazz Sethi, founder of the Diabesties Foundation, a patient support organization serving people with type 1 diabetes.
In addition to paying for healthcare supplies out of pocket, India has dramatic wealth inequality, which invariably impacts one’s diabetes management.
“Access to a good healthcare professional, to a hospital, to technology, to medication, depends purely on which household you were born into,” Sethi said in a presentation on socioeconomic barriers to diabetes care in the country.
The most basic supplies, test strips, insulin and needles, cost approximately $70 per month, according to Sethi.
A glucose monitor like the FreeStyle Libre can co $150 and supplies for an insulin pump can reach $100 per month. These costs are burdensome or far out of reach for many people with diabetes. The costs associated with diabetes supplies put individuals at risk of being inconsistent with their management protocols.
“A lot of money does not equate to good control. As long as we talk about affordability and money and access to technology, we need to also talk about access to good type 1 diabetes education,” she said. Sethi added she didn’t learn carb counting until about two years ago, despite living with T1D for 13 years.
Few people have access to comprehensive education and training on what diabetes is and how they can best manage it. For this reason, Diabesties Foundation focuses on peer support and education.
One program Diabesties runs is a phone-based education program called Back to Basics (B2B). Survey data demonstrated the following strengths and benefits of employing peer educators in the B2B program:

A survey of 350 participants demonstrated that over 70 percent of participants had little to no understanding of type 1 diabetes management before their B2B call.
And, most impressively, participants reported the following changes in A1C and hyperglycemia events after B2B training:
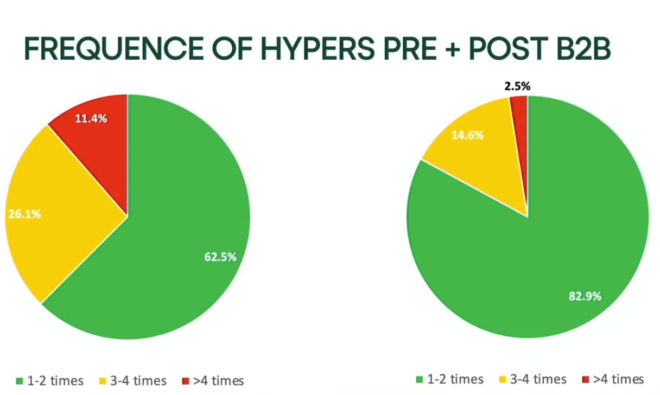
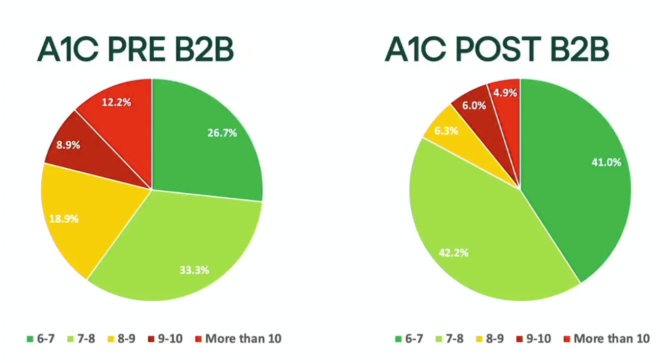
“We had cumulative A1c decreasing just because they could understand their condition more. This is no rocket science, right? It’s just understanding your patterns, understanding what works for you, learning things like carb counting,” Sethi said. “This is what happens when you just know a little bit more.”
Find more of Beyond Type 2’s coverage on ATTD 2022 scientific sessions.





