Lifestyle Interventions for Type 2 Diabetes Remission
Written by: T'ara Smith, MS, Nutrition Education
6 minute read
June 17, 2020
Type 2 diabetes remission is a hot topic within the T2D community. At the American Diabetes Association's 80th Scientific Sessions, researchers presented data on the impact lifestyle interventions had on the ability to achieve remission.
Editor’s Note: This article covers research presented at the American Diabetes Association’s 80th Scientific Sessions (ADA 2020) and is not an endorsement of a specific eating pattern. Before starting any new diet, please consult your healthcare provider.
At ADA 2020, researchers presented data on the impact of lifestyle interventions in order to achieve type 2 diabetes remission—a controversial subject in the type 2 diabetes (T2D) community. In the session, the presenters discussed the Diabetes Remission Clinical Trial (DiRECT) trial, low carbohydrate diets, and high fiber and plant-based diets to treat type 2 diabetes.
What is Type 2 Diabetes Remission? 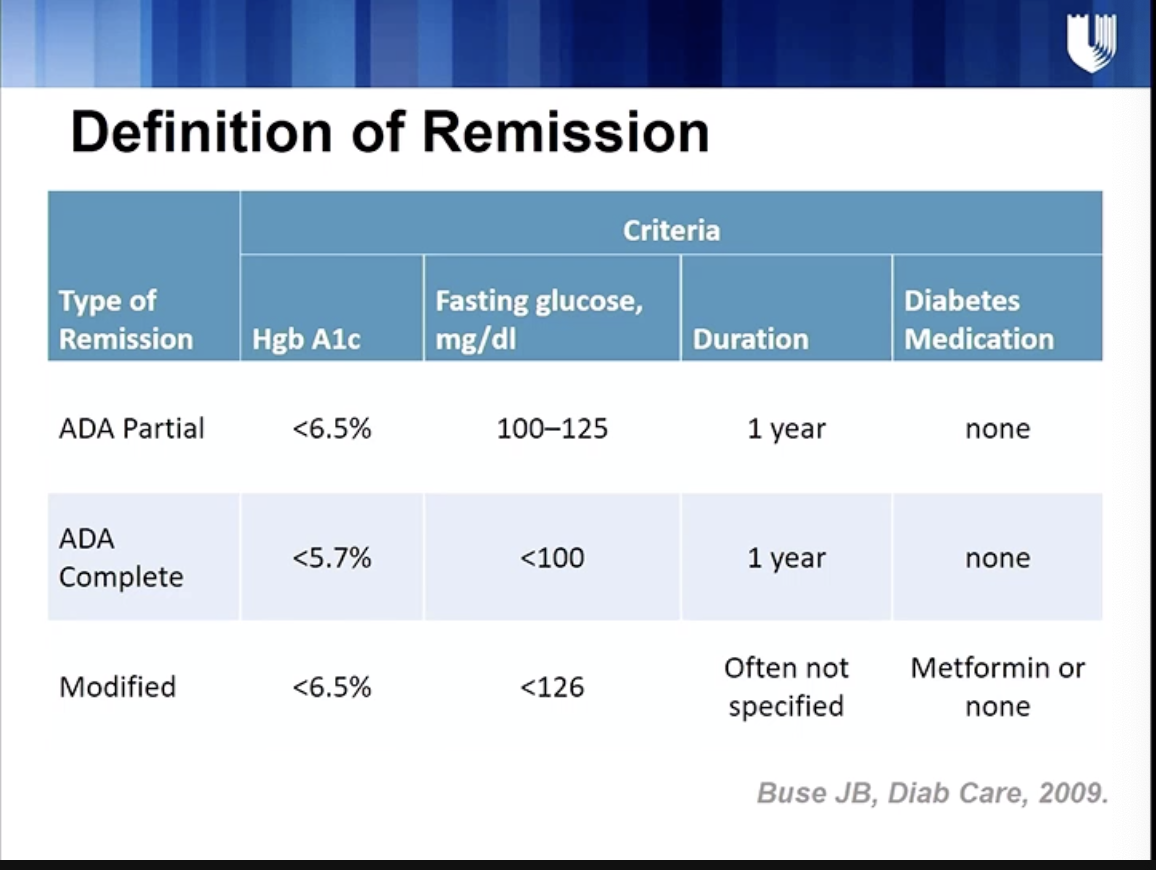
William Yancy, MD, from Duke Diet and Fitness, began the session by explaining that diabetes remission (as defined by the ADA) can be broken down into three types:
Partial Remission
Maintaining the following numbers for at least one year without diabetes medication:
- A1C of less than 6.5 percent
- Fasting blood glucose of 5.5-6.9 mmol/L100-125 mg/dL
Complete Remission
Maintaining the following numbers for at least one year without diabetes medication:
- A1C of less than 5.7 percent
- Fasting blood glucose of less than 5.5 mmol/L100 mg/dL
Modified Remission
While the duration to maintain these numbers isn’t often specified, modified remission is achieved with either the use of metformin or no diabetes medication. The additional criteria for remission are:
- A1C of less than 6.5 percent
- Fasting blood glucose of less than 7.0 mmol/L126 mg/dL
Achieving Diabetes Remission in the DiRECT Trial

The DiRECT Trial by Diabetes UK, Newcastle University and Glasgow University, studied the impact of a structured weight management program compared to the structured weight management program in people with type 2 diabetes who weren’t on insulin. The average age of the participants was 55 years old with an average body mass index (BMI) of 34.6. The population was also predominantly white and male.
Alison Barnes, RD, from Newcastle University discussed the lifestyle interventions people with diabetes in the DiRECT trial underwent to achieve diabetes remission.
At the beginning of the study, participants were put on a very low-calorie diet (VLCD) and were taken off diabetic medication and medication used to treat hypertension. A VLCD is a medically-supervised diet where an individual consumes about 800 calories or less per day. Initially all calories come in the form of meal replacement shakes. Over a period of months, patients are reintroduced to solid foods. Barnes gave some examples of why liquid diets are beneficial for those who aim to lose weight:
- Complete nutrition in fewer calories.
- Triggers for eating stand out, which is helpful when it’s time to reintroduce people back to normal foods and address those triggers.
- Easier to break and reform habits while creating a blank slate to improve eating habits
- Gives the individual a break from making eating decisions, a benefit especially for those who have complex relationships from food.
- Motivation from rapid weight loss. While it’s different than the motivation and satisfaction from gradual weight loss, liquid diets can help individuals stay motivated from the weight loss from a liquid diet.
Barnes also listed some potential side effects to liquid diets such as:
- Constipation
- Sensitivity to the cold due to the loss of body fat
- Dizziness as blood pressure begins to come down. At this point, the management of medications to treat hypertension must be addressed.
- For the first few days, individuals experience hunger and fatigue.
- Hypoglycemia. For people with diabetes, any blood glucose-lowering medications have to be managed and adjusted.
How do low-calorie diets achieve type 2 remission? Barnes cited the Twin Cycles of Type 2 Diabetes as potential explanation. The Twin Cycles hypothesis of type 2 diabetes states that type 2 diabetes is caused by excess fat in the liver and pancreas. In this process, the excess fat causes the liver to produce too much glucose. At the same time, the liver exports that extra fat to all of the body’s tissues, including the pancreas and within the pancreas, its function to produce insulin becomes impaired. To put type 2 diabetes in remission, the hypothesis claims the Twin Cycles must be reversed, specifically with a low-calorie diet and subsequently weight loss.

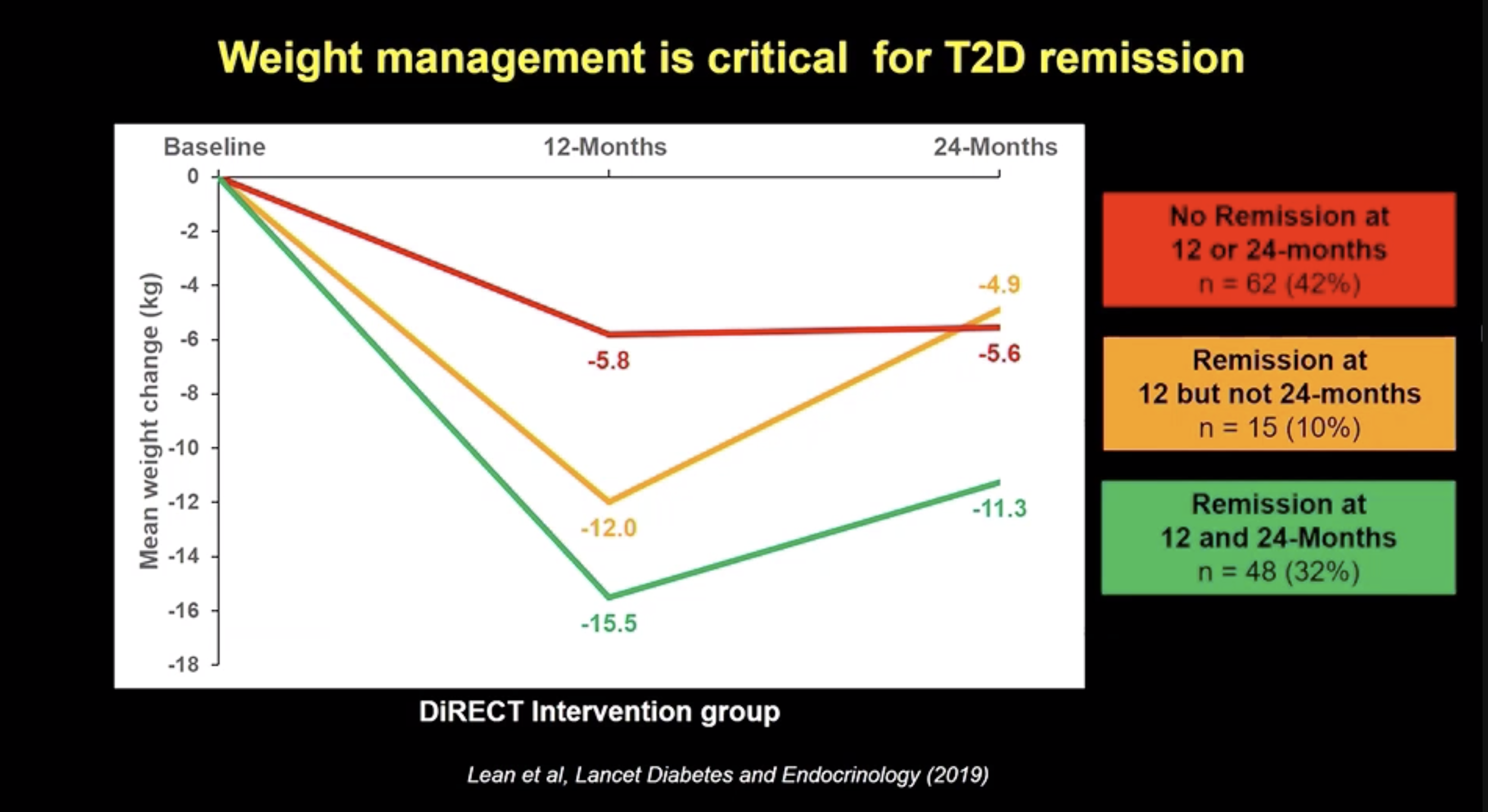
Data from the presentation showed diabetes remission was achieved and subjects on average maintained at least 10 kg (22 pounds) of weight loss. Also, Barnes emphasized remission may not be possible for every person with type 2 diabetes, depending on the progression of the disease, as the trial only included those who were living with diabetes for less than six years. The average length of time the participants were living with T2D was three years. Also, while the focus of the DiRECT trial is typically on the low-calorie intervention, the vast majority of resources are spent on helping participants maintain weight loss. Weight management was critical to maintaining remission at a 2-year follow-up. Barnes also noted type 2 diabetes symptoms will return if the weight is regained. Finally, other limitations to the study are its lack of ethnic diversity and how well these interventions could be conducted in a real-life setting.
What about Low-Carb and Plant-Based Diets? 
While the DiRECT Trial yielded some interesting results about the underlying mechanisms of type 2 diabetes and what it would take to put it into remission, other more familiar eating patterns were discussed, too, such as low-carb and plant-based eating.
Reporting on diabetes remission data from low-carb research is relatively new, according to Yancy. The doctor presented a 32-week study he conducted on 263 patients with type 2 diabetes, with an A1C of 8.0 percent or greater and a BMI of 27 or greater. Patients were placed in either of the below groups to track the impact on A1C.
- Shared Medical Appointment (SMA) Group: Participants in this group received diabetes education counseling, self-management training, and medication adjustments throughout the entire study.
- Weight Management and SMA: Participants in this group received low-carb diet counseling, self-management training, and medication adjustments for the first 16 weeks. For the latter 16 weeks, these patients received diabetes education counseling, low-carb diet support, continued self-management training, and continued medication adjustment.
Both groups saw significant decreases in their A1C, however, at the first 16 weeks, the weight management and SMA group saw a greater decrease in A1c. At a 48-week follow-up, both groups decreased by one percent. Yancy and his team also came up with a Medication Effect Score (MES) to determine how each group’s medication regimen changed over time. The weight management group saw a decreased use of medication, whereas the shared medical group increased their use of medication. Additionally, the weight management group lost more weight and 11 percent of them were able to achieve modified remission. To end his presentation, Yancy noted while low-carbohydrate diets are effective, it’s important for patients to receive close support from their doctors before starting a low-carb diet for weight loss.
Hana Kahleova, M.D., the Director of Clinical Research of the Physicians Committee for Responsible Medicine, highlighted the role a plant-based, high-fiber diet plays in diabetes remission, diabetes management and beta-cell function — the ability to regulate blood glucose through insulin production.
Compared to a regular diet with high-carbohydrates and saturated fat intake, a plant-based diet with unsaturated fat showed a decrease in insulin resistance and improvement of beta-cell function. Overall, Kahleova encouraged people with type 2 diabetes to eat a plant-based, high-fiber diet due to the decreased mortality risk from the disease.
While these studies showed that depending on the progression of the disease, type 2 diabetes remission may be possible with intense, medically-supervised interventions. However, it’s unclear how these treatments would work in a real-life setting. For people with type 2 diabetes, it’s important to consult with their health care team to decide what method of treatment would work best for their management plan.

Author
T'ara Smith, MS, Nutrition Education
T’ara was diagnosed with type 2 diabetes in July 2017 at the age of 25. Since her diagnosis, she focused her academic studies and career on diabetes awareness and living a full life with it. She’s excited to have joined the Beyond Type 1 team to continue her work. Two years later, T'ara discovered she'd been misdiagnosed with type 2 and actually has latent autoimmune diabetes in adults (LADA). Outside the office, T’ara enjoys going to the movies, visiting parks with her dog, listening to BTS and cooking awesome healthy meals. T’ara holds an MS in Nutrition Education from American University.
Related Resources

Already compatible with Dexcom’s G6 and G7 continuous glucose monitors (CGMs), the Omnipod 5 Automated...
Read more

The younger a person is diagnosed with type 2 diabetes, especially those with obesity, the...
Read more

The Oura Ring, which tracks things like sleep, heart rate, and activity, is joining forces...
Read more


