The Importance of CGM for Insulin-Dependent Type 2 Diabetes
This content was sponsored by Abbott, the makers of FreeStyle Libre 2,—a Founding Partner of Beyond Type 2.
It’s no secret people with type 2 diabetes sometimes have to use insulin to manage their blood sugar. Typically, it’s tracked using blood glucose meters (BGMs) which require fingersticks. With this method, you see what your blood sugar is in that snapshot of time. Is it high? Is it low? That’s what you’ll see. But there are some things BGMs don’t tell you—how your blood sugar is trending and how fast it’s rising or falling. To better understand the impact of insulin’s effects on blood glucose, a continuous glucose monitor (CGM) is a useful tool.
Here are some of the differences between BGMs and CGMs:
Blood Glucose Meters:
- Measures blood glucose directly to provide a single blood glucose reading
- Doesn’t require constant wear
- May be a less expensive option than a CGM
- Requires finger pricking, cleaning of the skin and a pricking technique to avoid pain
- Doesn’t show the trends of blood sugar ranges
Continuous Glucose Monitors:
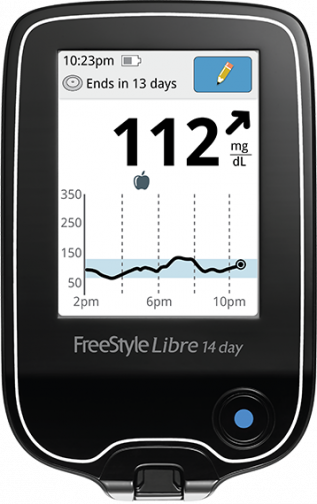
- Shows blood sugar trends over a period of time, and even at night
- Data can be shared with family/friends/HCPs
- Notifies you about high blood or low blood sugar events
- Gives you better data to adjust insulin dosages
- Painless way of checking blood sugar
 For people with insulin-dependent type 2 diabetes, the benefits of using CGM exceed the ones stated in the chart above. Wearing a CGM shows how factors other than your diet may have an impact on your blood sugar. You’ll be able to see the effects of factors like exercise, stress, or sleep.
For people with insulin-dependent type 2 diabetes, the benefits of using CGM exceed the ones stated in the chart above. Wearing a CGM shows how factors other than your diet may have an impact on your blood sugar. You’ll be able to see the effects of factors like exercise, stress, or sleep.
For diet-related fluctuations, you’ll be able to adjust more seamlessly if you can see trends in your blood sugar. Why trends? Let’s say you’re eating wheat toast one day and white toast another day. If you’re wearing a CGM, you may see the wheat toast steadily raises your blood sugar while the white toast raises it faster. Knowing more about what affects your blood glucose levels improves engagement in diabetes self-care and efficacy.
Knowledge Boosts Self-Empowerment
Have you ever been frustrated because your doctor’s visits have seemed unproductive and adjustments to your routine have been ineffective? If a big part of the problem is a lack of data and direction, a CGM can provide months’ worth of data. You can bring your data with you to appointments and work with your doctor to make changes to your diet, insulin dosages and more. There’s a feeling of empowerment people with type 2 diabetes get from knowing their own data as well as or better than their physician. Having the power to speak up about your own disease is an essential aspect of diabetes self-management. Remember: you’re the number one person on your healthcare team. Knowing your diabetes inside and out with the help of CGM data gives you the confidence to act like it.
Say Goodbye to Fingersticks
Those days of holding your breath and counting before pricking your fingers because you’re afraid of the pain? Say goodbye to them. Unless your CGM needs to be calibrated or if your CGM suggests you test using the traditional method, you won’t need to use a BGM. This relieves some of the anxiousness and stress associated with traditional blood sugar testing. As an insulin-user, pricking your fingers to check if your insulin dosages are correct seems exhausting. Using a CGM tells you in real-time how effective your current insulin-dosing strategy is, and does so painlessly.
Preventing Hypoglycemia
Insulin is a life-saving drug, but it’s also dangerous if used incorrectly or even correctly under certain circumstances. For example, insulin combined with exercise, alcohol, as well as a myriad of other factors can cause hypoglycemia or low blood sugar (<3.9 mmol/L70 mg/dL). Hypoglycemia, even mild cases, can have health consequences in the long run, including increased cardiovascular risks. Severe cases of low blood sugar can cause unconsciousness, cognitive impairment and even death. The goal for people with type 2 diabetes is to reach normal A1C levels without experiencing hypoglycemia. With the use of insulin to treat type 2 diabetes (T2D), rates of hypoglycemia rise. Some CGMs come with alerts to notify you when your blood sugar is dropping low. Others, such as the Freestyle Libre 14 day system, display a “Low Glucose” or “Glucose Going Low” message when you scan the sensor. Knowing this information can help you fine-tune your insulin therapy.
Reaching A1c Goals
Your A1c test should be completed at least every three months. But, to be honest, three months is too long to wait to learn from your doctor if you’re on the right track. Many go longer than three months and even a year without seeing a doctor. You should be able to know what’s working or not working sooner rather than later. In other words, you should know how much time you spend within your blood sugar target range.
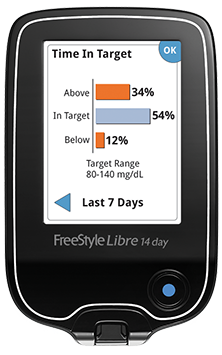
The standard range is between 3.9 mmol/L70 mg/dL and 10.0 mmol/L180 mg/dL. Ideally, you want to be within that range 70 percent of the time. Through traditional blood glucose monitoring, it’s tough to determine if you’re reaching that goal. The collective and real-time data from wearing a CGM shows you how much you’ve been within your range that day and over a period of time—like that three-month period between appointments. This gives you further flexibility within your diabetes routine. Knowing the correlation between time-in-range and A1c will likely remove some of the surprises from your bloodwork during your next appointment and you’ll have an idea about the progress of your A1c.
CGM as a Turning Point in Your Diabetes Care
A CGM for type 2s on insulin yields many benefits. CGMs are convenient, they’re painless, and they tell the story of your diabetes over a longer period of time. Having that extra information can empower you to use your voice confidently when speaking with your healthcare team. CGMs keep you engaged in learning about the many factors that impact your blood sugar. They give you the flexibility to make changes to your routine without waiting for your quarterly appointments with a doctor. And finally, they can help you reach your A1c goals safely by notifying you of possible low-glucose events. If you’re interested in getting started on a CGM, contact your healthcare provider.
Find more content pertaining to continuous glucose monitoring here.